Triheptanoin in Glucose Transporter Type 1 Deficiency
Hello Glut1 community!
I am so happy to share with you the latest publication by Dr. Juan Pascual and his team at UT Southwestern. The title of the publication is “Maximum dose, safety, tolerability and ketonemia after triheptanoin in glucose transporter type 1 Deficiency (G1D)”, which was published on March 1st in the Journal Nature, Scientific Reports. Everyone can access this article; it is open to the public and you can read it following this link.
While triheptanoin (C7) has been previously used in Glut1 deficiency, no work has established the ideal or maximum dose. Rather, a lower dose has been used based on experience derived from other uses. However, determining the highest safe and tolerable dose is important not only to achieve the maximum potential therapeutic benefit, but also to conduct rigorous research, since few conclusions can be reached when a treatment remains underdosed. In this manuscript, Dr. Pascual talks about the reasoning behind establishing a therapy for Glut1 Deficiency using triheptanoin (C7). He explains that in normal conditions, carbon enters the body with diet and exits as organic waste or respiration as CO2, and that carbon is used and refilled through different reactions which are necessary to sustain the brain metabolism. Glucose is broken down by a process called glycolysis and one of its products is a molecule called pyruvate. Pyruvate is necessary for cells to produce energy via a process called the tricarboxylic acid cycle or TCA. Pyruvate production depends on glucose availability in the body in this case, in the brain, therefore in Glut1 Deficiency where there is a reduction of glucose transported into the brain the amount of pyruvate produced as well as its derived products which are necessary for the TCA cycle are reduced, leading to encephalopathy or brain function alterations.
In the case of Glut1 Deficiency, some patients can be treated with a ketogenic diet and it is useful to treat some of their symptoms. However, Dr. Pascual explains that the main ketone products from the diet are not anaplerotic, which means that they cannot refill the intermediate molecules necessary for the TCA cycle. In addition, the diet also presents some side effects. These facts motivated Dr. Pascual and his team to study a therapy which could provide anaplerotic elements necessary for treatment of Glut1 Deficiency. With a clear picture of how the TCA cycle functions and the possible ways to supplement the missing anaplerotic elements that the ketogenic diet does not provide, he and his team decided to study the use of C7, the triglyceride of heptanoate to treat Glut1 deficiency patients. C7 provides a source for anaplerosis; in addition, previous studies by him and others had shown that C7 did not cause abnormalities in control individuals and that it could be beneficial in inherited lipid or carbohydrate metabolic disorders such as Glut1 Deficiency. The current study’s goal was to establish whether it was possible to treat children with Glut1 Deficiency with a higher dose of C7 than previously studied and to determine the safety, tolerability to the maximum tolerated dose (MTD) as well as to determine the potential of C7 to produce byproducts that are anaplerotic.
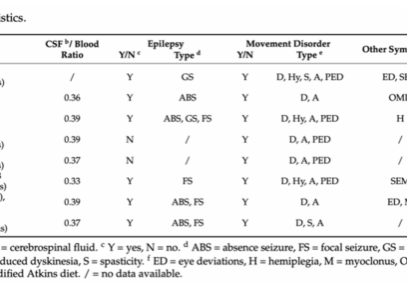
The current study enrolled patients who had participated in previous C7 clinical studies done by Dr. Pascual and his team at the Rare Brain Disorders Program of UT Southwestern, and additional patients, and were separated by age groups. The patients enrolled in the study had a confirmed Glut1 Deficiency diagnosis by genetic testing or by a brain fluoro-deoxyglucose positron emission tomography (PET), and were either on a regular diet or a modified Atkins diet.
Treatment:
The approach used an innovative design previously proven very successful in cancer dose-finding studies. This design had not been previously used in neurological studies. The main advantage is that this resulted in efficient and precise dose-finding using a much more limited number of patients relative to other methods. Patients were separated into 3 groups according to age. Patients underwent physical and neurological examinations as well as a nutritional assessment to estimate their average daily calories consumed. Moreover, patients had blood work to measure different metabolites as a baseline. Then patients received the C7 dose between 35% and 45% of their daily caloric intake; the dose of C7 oil administered was divided into 4 doses per day and it was administered before meals during 7 days. Dr. Pascual’s team measured tolerance to C7 during those days, patients had a physical examination, and a tolerability and toxicity assessment every 2-3 days. Physical examination, blood work and tolerability and toxicity studies were performed on two different days after the C7 administration had ended on day 7. Follow-up assessments of side effects were done a month after C7 administration had ended via telephone.
In a separate group of patients, a different schedule of C7 administration was established. Patients also received baseline blood work assessment and physical examination. The purpose of the study with this group of patients was to determine the type of ketone bodies being produced as a result of C7 intake and to establish whether anaplerotic products were being produced.
Results:
According to Dr. Pascual and his team, some of the patients in both groups experienced gastrointestinal discomfort which lessened when the dose was reduced and then gradually increased to the desired level. Overall, the patients’ blood work showed no significant differences before and after C7 consumption. One patient had a seizure during the study which was consistent with his history and severity of epileptic episodes.
The results from the studies indicate that the maximum tolerated dose of C7 in all the patient groups did not depend on the age of the patient, as it was similarly tolerated for all ages. In addition, the concentration of the anaplerotic product produced from C7 oil varied across all patients. Furthermore, their results suggest that ketones produced from the ketogenic diet or a regular diet compared to the ones produced from C7 oil are made from different metabolic processes. Dr. Pascual and his team state that C7 oil is advantageous over just a dietary treatment because it could be combined with a regular diet or a modified Atkins diet, allowing for a balanced diet. Additionally, he explains that patients with non-epileptic forms of Glut1 Deficiency and young babies continue to be diagnosed, therefore simpler diets would be better accepted for their treatment. However, more studies need to be done to establish the possible combination of C7 with the ketogenic diet.
Conclusion:
Dr. Pascual and his team concluded that C7 oil provides an anaplerotic alternative to the ketogenic diet treatments. In addition, they concluded that C7 oil dose at 45% of the patient’s daily caloric intake is safe despite the initial period of frequent gastrointestinal issues. Their future work will characterize the efficacy of C7 oil, its long-term use, safety and tolerability and its compatibility with the ketogenic diet.
Thank you to Dr. Pascual for taking the time to review this document!
If you have any questions or comments please feel free to email me to [email protected]
Thank you for visiting our blog!